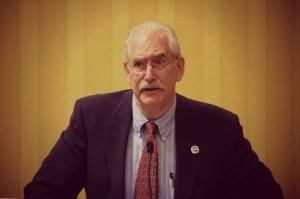
 Join Together recently spoke with R. Jeffrey Goldsmith, MD, DLFAPA, FASAM, the President of the American Society of Addiction Medicine, about Obamacare and the state of addiction treatment.
Join Together recently spoke with R. Jeffrey Goldsmith, MD, DLFAPA, FASAM, the President of the American Society of Addiction Medicine, about Obamacare and the state of addiction treatment.
How has Obamacare changed the practice of addiction medicine?
Dr. Goldsmith: It hasn’t dramatically changed the practice of addiction medicine yet, but its promotion of integrated and coordinated care systems has set the stage for addiction medicine to be delivered as part of mainstream medical care rather than “carved out” or available only in specialized settings. It will still take quite a bit of time for these changes to take root on a broad scale. But we are hearing more conversations about care coordination and seeing some pilot programs that are working to integrate addiction treatment services into care models such as Patient-Centered Medical Homes, which were promoted in the law. It was pointed out to me that about 50 percent of the physicians in mental health care are avoiding insurance and require cash payments. This is an end-run around Obamacare and may speak to the many ways of putting up quiet barriers like “approval of medication- assisted treatment” before it is covered.
What changes does ASAM still want to see?
Dr. Goldsmith: ASAM would still like to see greater enforcement of the Mental Health Parity and Addiction Equity Act, which was passed in 2008 and expanded upon through the Affordable Care Act. The final regulations for commercial plans weren’t released until 2013 and we are still waiting on final regulations for Medicaid Managed Care Organizations. Because it is not being enforced strongly, there are still major violations. We need greater clarity and direction from the Obama Administration on what plans need to disclose to patients and more transparency about violations and investigations. It won’t have its intended effect until it is properly enforced.
We’d also like to see greater efforts taken to expand the addiction treatment workforce. There are far too few specialists to meet the demand for treatment, and most health care professionals – physicians and allied health care providers – receive little to no education on substance use disorders as part of their training. One way to address this training limitation is to have good inter-professional collaboration. One specialist can help a multidisciplinary team manage a large patient population. This kind of collaboration requires honoring everyone in the team, seeking their information about the patient and opinions about addictions, setting up regular opportunities to talk with each other, and have skills for leading and skills for following the Team Leader. We need medical and nursing schools to add this addiction and inter-professional collaboration education to their curricula. Furthermore, we need funding for more residency and fellowship spots for those doctors who want to specialize in addiction medicine.
ASAM has helped Hazelden/Betty Ford create teaching resources that all medical schools can lease to use for teaching students and residents, and bringing faculty up-to-date on state-of-the-art addiction care. It is called the CARE project. In parallel to this action, we need more national guidelines for good addiction care, both pharmacotherapy and the use of evidence based psychotherapy. Without these, different professional groups choose their own preferences and ignore the research evidence that can be quite strong in these treatment areas. This can interfere with good inter-professional collaboration and the payer’s belief that there is effective care upon which everyone agrees.
Finally, we need greater reimbursement for addiction treatment services, which will expand access immediately by incentivizing physicians to offer these services and incentivize students to enter the field. Too often, commercial insurers and state Medicaid programs do not pay physicians enough to make it worthwhile for them to offer these services. Physicians must choose between seeing patients at a loss, charging patients cash, or exiting the field altogether.
Why are so many people still not receiving addiction treatment, although they need it?
Dr. Goldsmith: In addition to the reasons discussed above – lack of enforcement of parity, a short workforce supply, and poor payment for treatment services – stigma still plays a major role in dissuading patients from seeking treatment and preventing health care providers from offering it. We know that stigma can:
- Discourage individuals from seeking help.
- Reinforce the idea that someone with a substance use disorder is exhibiting a willful choice rather than suffering from a recognized medical condition which continues for years.
- Evoke less sympathy and empathy that would happen if the individual is understood to have a disease.
As long as patients, providers, family members and friends continue to view addiction as something other than a prolonged disease for which medical treatment is available, there will continue to be a treatment gap. It is important to see that the public stigma about addiction triggers and reinforces the internal, unconscious stigma that each person carries around. People don’t want to see themselves as out of control, or weak. They need to see the biological aspects of the disease to drop their own unconscious disparaging stigma. This affects the individual, the family and the community. Working on one segment will help the others grow and improve.
R. Jeffrey Goldsmith, MD, DLFAPA, FASAM, is the President of the American Society of Addiction Medicine.
Published
December 2015
 Get Support
Get Support
